Answered: What Is the Most Painful Type of Neuropathy?

Living with neuropathy can be overwhelming, especially when the pain is severe. Neuropathy affects the peripheral nervous system, the network connecting the brain and spinal cord to the rest of the body. When these nerves are damaged, it can lead to intense discomfort, limiting one’s ability to perform daily tasks.
The most painful types of neuropathy—such as trigeminal neuralgia, diabetic peripheral neuropathy, and postherpetic neuralgia—cause severe pain that disrupts physical and emotional well-being. This article provides a comprehensive look at these types, their symptoms, and effective ways to manage them.
Key Takeaways
- Most Painful Types of Neuropathy: Trigeminal neuralgia, diabetic peripheral neuropathy, and postherpetic neuralgia are among the most painful types, each causing intense and often debilitating pain.
- Symptoms to Watch: Common symptoms include burning, stabbing, or electric shock-like pain. Trigeminal neuralgia affects facial nerves, diabetic neuropathy impacts legs and feet, and postherpetic neuralgia causes lingering pain after shingles.
- Treatment Options: Effective management includes a combination of medications, physical therapy, lifestyle adjustments, and, in some cases, surgical intervention. Techniques like TENS can provide targeted relief.
- Lifestyle Modifications Matter: A balanced diet, regular exercise, and avoiding alcohol can support nerve health and improve symptom management.
Critical Types of Painful Neuropathy
When considering the most painful neuropathies, several conditions stand out due to their intensity and the toll they take on daily life. Below, we identify the three most painful types.
Dr. Evan Norum, a board-certified chiropractor specializing in neuropathy, states, “The most painful types of neuropathy often stem from conditions like diabetes, shingles, and specific nerve compression issues. These types are relentless and can deeply affect a person’s quality of life.”
| Neuropathy Type | Pain Description | Common Symptoms |
|---|---|---|
| Diabetic Peripheral Neuropathy | Burning, stabbing, or tingling pain, often in feet and legs | Muscle weakness, foot ulcers, dizziness, numbness |
| Trigeminal Neuralgia | Electric shock-like, sudden facial pain | Triggered by light touch, brushing teeth, facial movement |
| Postherpetic Neuralgia | Lingering burning pain, sensitivity to touch | Follows shingles, pain persists long after rash heals |

Diabetic Peripheral Neuropathy
Diabetic peripheral neuropathy primarily affects people with diabetes, damaging nerve fibers in the legs and feet. The pain can be severe, characterized by burning, stabbing, or tingling sensations that make walking difficult or performing daily tasks difficult. In addition to pain, complications can include foot ulcers and dizziness due to blood pressure changes.
“Managing diabetic neuropathy is critical for preserving mobility and avoiding complications,” explains Dr. Taylor Moore, a board-certified in neuropathy. “In our practice, we focus on managing blood sugar levels and using targeted therapies to address nerve pain directly.”
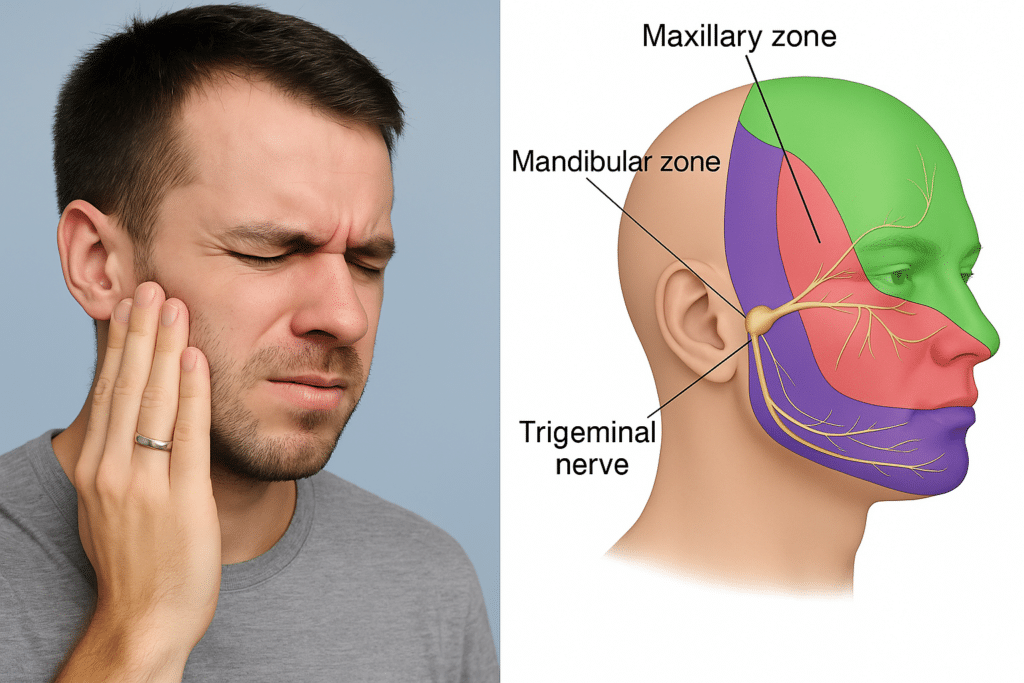
Trigeminal Neuralgia
Known as one of the most excruciating forms of neuropathy, trigeminal neuralgia (TN) involves intense facial pain. This condition affects the trigeminal nerve, which is responsible for facial sensations. It can cause sudden, sharp pains that feel like electric shocks. Actions as simple as brushing teeth or exposure to a breeze can trigger these painful episodes, impacting mental health and quality of life.
According to Dr. Norum, “Trigeminal neuralgia can be devastating for patients. Even slight movements or touches can set off severe pain, making daily life incredibly challenging. Medications and, in some cases, surgical intervention are essential in providing relief.”

Postherpetic Neuralgia
Postherpetic neuralgia (PHN) often follows a shingles outbreak and occurs when the varicella-zoster virus damages sensory nerves. This condition leaves individuals with lingering pain that can last months or even years after the initial shingles rash has healed. Many describe the pain as burning or stabbing, with heightened sensitivity that makes even light touches unbearable.
“Postherpetic neuralgia is a difficult condition to manage because it follows the nerve damage left by shingles,” Dr. Moore says. “Our goal in treatment is to minimize pain through medication, nerve blocks, and lifestyle adjustments to improve quality of life.”
What Makes These Types So Painful?
Several factors contribute to the high pain levels associated with these types of neuropathy. In diabetic peripheral neuropathy, elevated blood sugar damages nerves, leading to painful sensations that worsen over time. Trigeminal neuralgia’s pain is amplified by the sensitivity of facial nerves, and postherpetic neuralgia’s lingering pain is due to ongoing nerve damage even after the shingles virus has healed.
These types often involve damage to the peripheral nervous system, critical in relaying sensory information to the brain. When these nerves are damaged, they can misinterpret or amplify standard signals, leading to persistent or exaggerated pain.
Causes and Triggers of Severe Neuropathic Pain
Understanding what causes severe neuropathy pain can help manage symptoms more effectively. Key causes include:
- Diabetes Complications: High blood sugar levels can damage nerve fibers, leading to diabetic peripheral neuropathy, which is one of the most painful conditions.
- Nerve Compression or Trauma: Injuries from repetitive movements or physical trauma can lead to nerve compression syndromes, such as carpal tunnel syndrome.
- Viral Infections: Viruses like shingles and herpes simplex damage nerves, leading to conditions like postherpetic neuralgia, which causes chronic nerve pain.
These factors, whether related to chronic diseases or physical injuries, contribute to the heightened sensitivity and pain associated with neuropathy.
Recognizing Symptoms of Severe Neuropathy
Neuropathy pain varies widely depending on the type. Common symptoms among painful types of neuropathy include:
- Burning or Freezing Pain: Common in diabetic peripheral neuropathy, this sensation feels like walking on hot coals or ice shards.
- Sudden, Stabbing Pain: This sensation is prevalent in trigeminal neuralgia and often resembles a sudden electric shock in the face.
- Chronic Throbbing Pain: A persistent dull ache, often in postherpetic neuralgia, disrupts sleep and daily activities.
As Dr. Norum notes, “Recognizing these symptoms early is crucial for managing neuropathy. By identifying specific pain patterns, we can better target treatments to relieve discomfort and improve function.”

Treatment Options
Treatment for neuropathy pain includes a combination of medication, physical therapy, and lifestyle changes. Below are the primary treatment methods and approaches.
Medications
Doctors commonly prescribe antidepressants (like amitriptyline) and anticonvulsants (such as gabapentin) for nerve pain. These medications alter how the brain processes pain signals, offering some relief. Topical treatments, including capsaicin cream and lidocaine patches, can target localized pain, particularly in postherpetic neuralgia.
Physical Therapy and TENS
Physical therapy is often recommended to improve mobility and strengthen affected areas.
Dr. Moore shares, “In our practice, we use techniques like transcutaneous electrical nerve stimulation (TENS) to help reduce pain by interrupting pain signals to the brain. Physical therapy can improve blood flow and reduce inflammation, offering significant relief.”
Surgical Options
For severe cases, surgery may be necessary, particularly in trigeminal neuralgia. Options include nerve decompression or even severing problematic nerves to reduce chronic pain. Patients with carpal tunnel syndrome may also benefit from surgical intervention to alleviate nerve compression.
Lifestyle Modifications
Adjusting lifestyle habits can significantly help in managing neuropathy pain. Here are some suggested lifestyle changes:
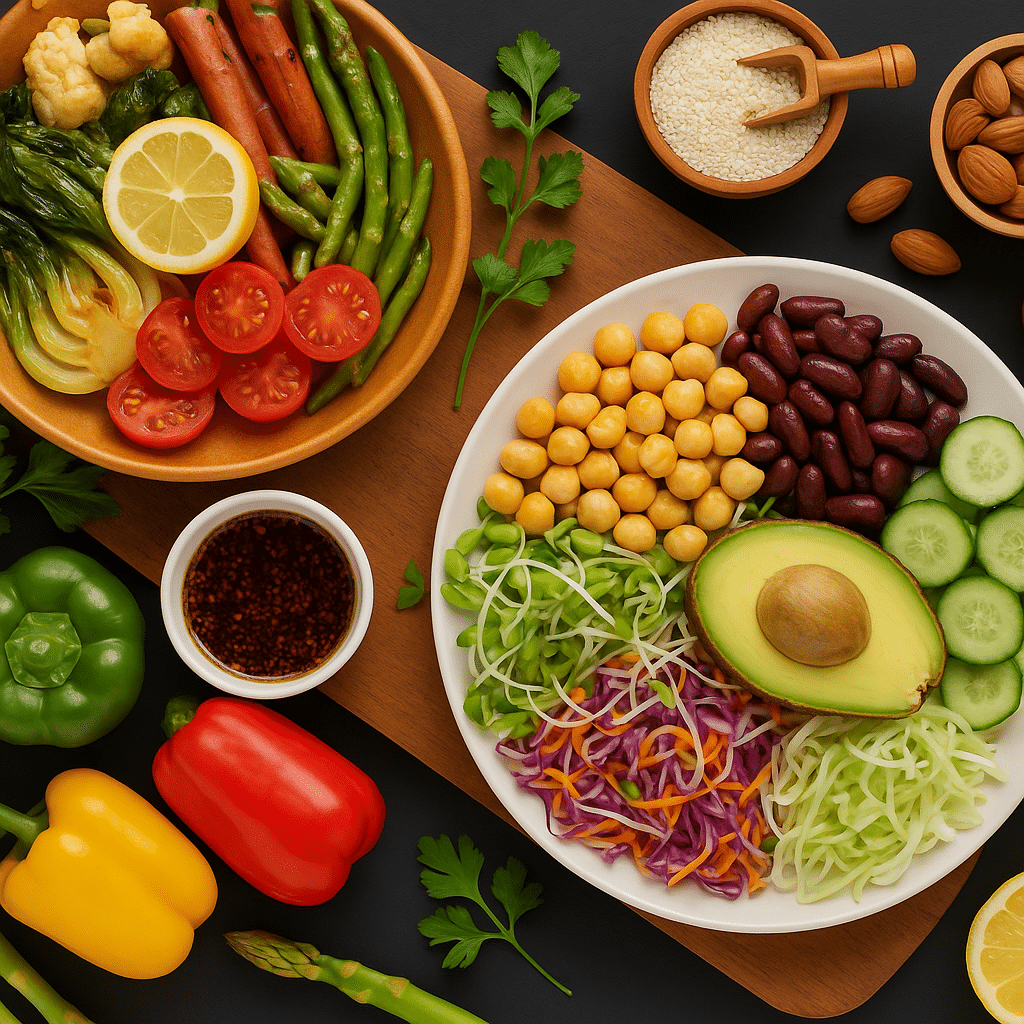
- Balanced Diet: A diet rich in fruits, vegetables, lean proteins, and whole grains promotes nerve health. Reducing sugar intake is crucial for those with diabetic neuropathy. Read our complete guide on foods to avoid with neuropathy.
- Regular Exercise: Gentle activities like walking and swimming can improve circulation and reduce pain. Avoiding alcohol is also important, as it can exacerbate nerve damage.
Dr. Norum adds, “We emphasize a holistic approach to neuropathy treatment. Lifestyle adjustments and medical interventions provide a foundation for effective pain management and improved quality of life.”
Conclusion
Peripheral neuropathy’s most painful forms—diabetic peripheral neuropathy, trigeminal neuralgia, and postherpetic neuralgia—require dedicated management due to their intensity and impact on daily life. While each type brings unique challenges, identifying the symptoms and understanding treatment options can empower you to take control.
As Dr. Moore recommends, “Don’t let neuropathy define your life. By seeking the right treatments, adjusting your lifestyle, and working with a healthcare provider, you can improve your quality of life and manage pain more effectively.”
If you or someone you know is struggling with neuropathy, consider consulting a board-certified chiropractor or a healthcare provider to discuss tailored solutions for relief.
FAQs
What is the most painful type of neuropathy?
Among the painful neuropathies, trigeminal neuralgia, diabetic peripheral neuropathy, and postherpetic neuralgia are known for their intensity. Each of these types affects sensitive nerve areas, resulting in severe pain.
How can I manage neuropathy pain?
Effective neuropathy management often combines medication, physical therapy, and lifestyle changes. Consult with a healthcare provider to develop a tailored treatment plan.
What causes neuropathy pain to worsen?
Triggers like elevated blood sugar, physical injury, or viral infections can aggravate neuropathy pain. Working with a healthcare provider can help control these triggers and manage pain.

About the Author
Dr. Evan Norum, co-owner of Advantage Chiropractic in New Berlin, WI, holds a Doctorate of Chiropractic from Northwestern Health Sciences University. Inspired by personal experiences with chiropractic care, he specializes in family-based treatments and is board-certified in chiropractic care, neuropathy, and the Torque Release Technique®. With internships at leading chiropractic centers and co-founding Advantage Chiropractic in 2017, Dr. Evan Norum is dedicated to promoting health from within.
